TIME published a story this week looking at data that shows how drastically the risk of COVID-19 infection varies from neighborhood to neighborhood within Boston.
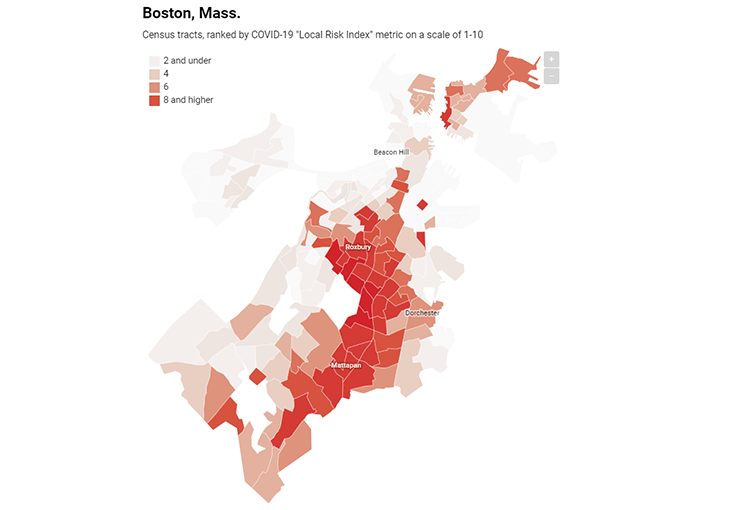
Using data from the City Health Dashboard, a project run by New York University Langone Health, TIME mapped Boston and its neighbor across the Charles River, Cambridge, to illustrate how significantly socioeconomic profiles can affect risk of disease.
The map shows how the Boston neighborhoods of Roxbury, Mattapan, East Boston and Dorchester have much higher risk of COVID-19 infection than other areas of Boston. Cambridge has low risk of infection citywide.
Cambridge has a significantly higher median household income than Boston ($95,000 vs. $66,000) and fewer residents living in poverty (13% vs. 20%), according to the U.S. Census Bureau.
From the TIME article:
Take Boston. The city has long struggled with racial and income inequity, and that’s clearly reflected in its COVID-19 risk spectrum. Residents of wealthy neighborhoods, like Beacon Hill and the Back Bay, can leave their homes each day with relative confidence they won’t get sick, while people in poorer, predominantly Black and Hispanic neighborhoods, like Roxbury, Dorchester and Mattapan, are at much higher risk.
The COVID-19 pandemic has unmasked long standing racial and ethnic health-related disparities, according to a study in the American Heart Association journal Circulation. Higher rates of COVID-19 hospitalizations, deaths or positive cases among blacks, Hispanic/LatinX and Native Americans are being reported at local and national levels.
The health disparities exposed by the current public health crisis did not materialize in a vacuum but are largely driven by socio-economic and environmental factors, according to the study. The emerging differences in COVID-19 complications by race/ethnicity are being driven, in part, by a higher prevalence of one or more pre-existing chronic health conditions such as hypertension, type 2 diabetes and kidney disease at an earlier age among U.S. minorities.
Moreover, social distancing is difficult in impoverished communities because of overcrowding, residence in multigenerational households, and the inability to work from home, the study found.