Nearly 30% of residents in the Greater Richmond region have high blood pressure. High blood pressure (hypertension) is a major risk factor for heart disease and stroke. Further, the impact of the COVID-19 pandemic has exacerbated food insecurity, yet good nutrition and blood pressure (BP) control go hand in hand. In the region, food pantries have seen a significant increase in utilization during the height of the pandemic and individual pantries are averaging 500-1000 households per year, the majority of which are Black and/or Hispanic, and 100% low income.
One of the ways the American Heart Association is addressing health inequities is to decrease rates of hypertension by collaborating with organizations that serve those who are low-income, uninsured, or underinsured. With community organizations addressing food insecurity, we advocate for nutrition guidelines that reduce sodium and increase access to fresh produce for those experiencing barriers to nutritious foods. With healthcare providers, the Association provides information and resources to increase accurate BP measurement, treatment, and the empowerment of patients.
Through a community BP program, the American Heart Association, Feed More, Capital Area Health Network (CAHN), and the Richmond and Henrico Health District Medical Reserve Corps have come together to further reach underserved populations and increase access to the resources needed to reduce nutrition insecurity, uncontrolled hypertension, and lack of access to care. With a laser focus on evidence-based strategies and sustainability, AHA is working with these community and clinical organizations to implement self-measured BP monitoring (SMBP) programs. SMBP enables physicians to better diagnose and manage hypertension while supporting patients to take an active role in their BP control. Working within community settings such as food pantries, we can better meet people where they are to increase their access to care.
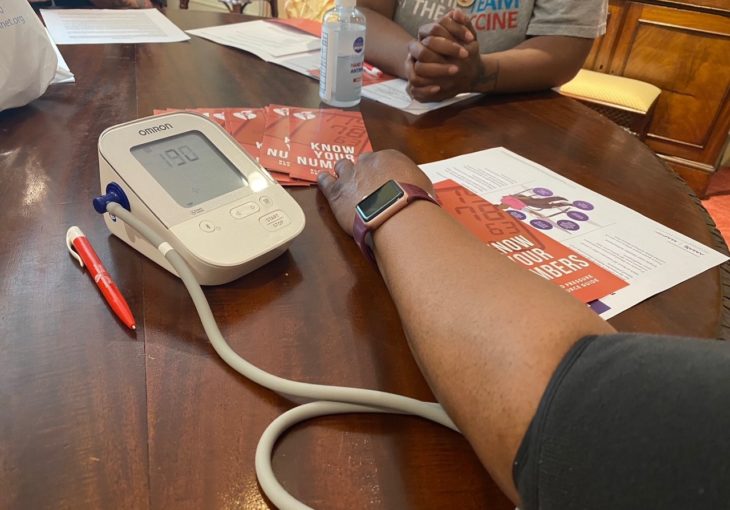
As the Central Virginia area’s food bank, Feed More is working to implement a Wellness Pantry model at pantries across the Greater Richmond region. Wellness Pantries are centered on client choice, which includes shopping for items to increase dignity while also incorporating healthy nudges and labeling that promotes more nutritious items such as those with lower sodium, whole grains, proteins, and fruits and vegetables. AHA approached Feed More about collaboration to implement regular BP screenings at their wellness pantry sites and include clinical referrals to help participants access validated blood pressure devices. Launched in May 2022, St. Stephen’s Episcopal Church, St. Thomas Episcopal Church, HandUp Resource Center, and Chesterfield Food Bank & Outreach Center have championed BP screenings to be held on a regular, monthly basis with the potential to reach over 1,000 people a month.
Capital Area Health Network (CAHN) provides affordable and quality healthcare in six health centers centered on culturally responsive patient care, education, and advocacy to promote health and quality of life for all residents in Metropolitan Richmond. CAHN serves approximately 13,920 patients, the majority of which are Black/African American, Hispanic/Latinx, and low-income. CAHN has the community at heart and has been a significant partner to the American Heart Association in creating a clinical linkage for those with uncontrolled high BP. In spring 2022, CAHN began implementing a patient self-measured BP (SMBP) program in all of their locations. Patients appropriate for SMBP include those who receive a BP screening whose measurements appear elevated in the Wellness Pantries. Research has shown that self-monitoring, coupled with clinical support, enhances the accessibility of care, and improves BP control.1 The launch of their SMBP program was made possible by a grant as a result of the national partnership with AHA and Quest Diagnostics. CAHN was selected as one of ten sites across the U.S. to invest resources in in order to double down on BP control in underserved communities.
The Association provided each Wellness Pantry with a BP toolkit that included two validated blood pressure monitors/cuffs, patient education resources, and personal protective equipment. In collaboration with the Richmond and Henrico Health District, volunteers from their Medical Reserve Corps will conduct the four monthly screenings. AHA also conducted training for Wellness Pantry site staff and medical volunteers to implement the community BP program, which included training on the need for and importance of BP control and how to support participants in measuring accurately at home. Through the community initiative, access to BP monitors will allow for accurate readings and documentation in the patient’s medical chart to support hypertension control regardless of who engages with the patients at Wellness Pantries. Medical volunteers not only take BP measurements, but teach participants how to measure accurately at home, record their measurements, and share their numbers with their healthcare team. After the first year of the program, Feed More hopes to embed BP screenings and education throughout their programing including all Wellness Pantry sites.