According the American Stroke Association, a division of the American Heart Association, depression is a common experience for stroke survivors. A scientific statement from the Association indicates that about one-third of stroke survivors experience depression – compared to 5%–13% of adults without stroke. If left untreated, it can affect quality of life and make post-stroke recovery more difficult.
According to statements from his office, Sen. John Fetterman, who had a stroke in May of 2022, has sought in-hospital treatment for depression, resulting in media and public inquiries related to stroke and depression.

“Having a stroke is a very large, significant, devastating life event, and often acute depression occurs after those type of events, for example if you’re involved in a car crash,” said Dr. William W. Ashley Jr., the Director of Cerebrovascular and Endovascular Neurosurgery at LifeBridge Health in Maryland.
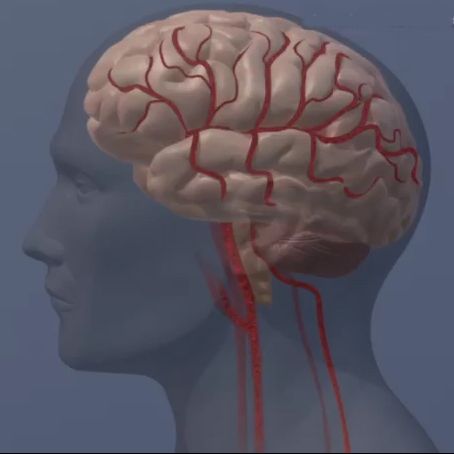
“In addition, stroke affects the brain chemistry, including the frontal lobes and limbic system, as well as neuroinflammation after a stroke,” all of which can lead to symptoms of depression, he said.
Ashley, who is also president of the American Heart Association/American Stroke Association Baltimore & Greater Maryland board of directors, suggests stroke survivors who experience depression seek evaluation and treatment with a qualified professional.
“It’s important to recognize the signs of depression, which can include a feeling of emptiness or being disconnected, apathy, sleeping problems, physical manifestations such as a lack of appetite, and suicidal thoughts,” Ashley said.
Because stroke can disrupt sleep, eating, continence and other bodily functions, self-care is critical including reaching out to friends and family for emotional support and to overcome any stigma associated with seeking help.
Unfortunately, because both stroke and depression still carry social stigma and shame, many stroke survivors are reluctant to seek help and may need extra support to acknowledge the symptoms of depression and seek treatment.
“Many times people can’t get understand why they feel this way after a stroke,” Ashley said. “The message here is it’s a normal outcome, not something to be embarrassed or concerned about.”
As with all forms of depression, a combination of counseling, medication, stress-reduction, and regular exercise can all be helpful. Because depression is a serious health condition, treating it promptly and effectively is vital. Treating depression not only improves mood, but it also boosts physical, cognitive and intellectual recovery. Several studies show that depression goes hand in hand with lower levels of social support. Support from family, friends, a stroke support group or a combination of resources can be beneficial for a stroke survivor’s mental long-term wellbeing and can be an important part of a treatment plan for post stroke depression.
“You would feel normal about getting treatment after breaking your leg, it’s normal to get this kind of treatment after a stroke, and there are a lot of resources and support groups available to help patients and families address these feelings of depression, including the American Heart Association,” Ashley said.
The American Heart Association has a Support Network for patients, families and caregivers than can help stroke survivors battling depression – www.supportnetwork.heart.org.
Here are some of the common symptoms of depression, according to the Association:
- Persistent sad, anxious or “empty” mood
- Restlessness and irritability
- Feelings of hopelessness, pessimism, guilt, worthlessness or helplessness
- Loss of interest or pleasure in hobbies and activities, including sex
- Decreased energy and fatigue, and feeling “slowed down”
- Difficulty concentrating, remembering and making decisions
- Insomnia, early-morning awakening or oversleeping
- Appetite and/or weight changes
- Thoughts of death or suicide, or suicide attempts
According to the American Stroke Association, stroke is the No. 5 cause of death and a leading cause of disability in the United States.
Stroke can happen to anyone — any age, any time — and everyone needs to know the warning signs. Calling 911 alerts first responders who may start treatment on someone experiencing stroke symptoms before arriving at the hospital. Use the letters in F.A.S.T to spot a stroke:
- F = Face Drooping
- A = Arm Weakness
- S = Speech Difficulty
- T = Time to call 911
Beyond F.A.S.T. – other symptoms you should know:
- Sudden NUMBNESS or weakness of face, arm, or leg, especially on one side of the body
- Sudden CONFUSION, trouble speaking or understanding speech
- Sudden TROUBLE SEEING in one or both eyes
- Sudden TROUBLE WALKING, dizziness, loss of balance or coordination
- Sudden SEVERE HEADACHE with no known cause
Additional resources